Easy Does It, a non-profit organization founded by people with disabilities in 1994, provides emergency personal assistance services, accessible transportation, wheelchair and assistive device repair, case management and other services for people with physical disabilities who live in Berkeley, California. In 2018, with 26 employees and a $1.2 million budget, EDI responded to 3,814 requests for service from about 600 disabled and older residents of Berkeley.
Reports & Publications


This brief outlines a proposal for an innovative program that assists states with improving their home and community-based services (HCBS) infrastructure. Key goals include strengthening housing, transportation, employment, workforce and caregiver supports in communities across the country with initiatives that address social determinants of health (SDOH), so that persons with disabilities and older adults with disabilities are served where they wish to be served.
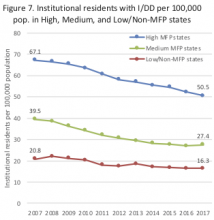
Since 2007, states with Money Follows the Person (MFP) programs transitioned more than 90,000 people receiving long-term services and supports in institutions back to their homes and communities.
Objectives: To explore the effect of the Affordable Care Act (ACA) on disparities in access to health care based on disability status, as well as age, income, race, and ethnicity.
During the Community Living Summit held on May 3-4, 2018, the participants came up with a lot of questions about studying autism and living in the community. After the Summit, ASAN thought about what they said and then came up with some more questions.
Together, we came up with seven big questions:
1. How can we help autistic people live in the community?
2. What is the autistic community like?
3. How should we study autism?
4. How can we help autistic people stay on track?
5. Where should autistic people live?
